Guided Tissue Regeneration (GTR)
Case Summary: Guided Tissue Regeneration (GTR) is a technique performed to promote osseous regeneration, allowing for tissue growth (bone and soft...
Stomatitis refers to widespread inflammation of the mucous lining of the mouth's structures, often associated with an underlying immune system issue. This painful condition manifests with ulcerated and friable gums, extending to the caudal mouth in severe cases. True feline chronic gingivostomatitis (FCGS), or stomatitis, always involves caudal mouth inflammation and commonly coincides with tooth resorption and periodontal disease.
Full mouth extractions (FME) are necessary for ALL cases with caudal mouth inflammation, with 67-90% of cats responding well to FME, while the remaining may require extended medical management. A better outcome is achieved when extractions are performed as first line treatment and occur earlier in the course of disease. The longer patients are on medical management prior to full mouth extractions the less likely of a curative outcome after full mouth extractions.
In this case, the patient presented to RDVM, Dr. Amanda Miller, of AMVC Veterinary Clinic, with caudal mouth inflammation. Owner noted halitosis in March of 2023, and caudal mouth inflammation was found at anesthetic dental procedure with their referring DVM in April of 2023.
MN 8yo DSH. History of abnormal eating habits, excessive drooling, and halitosis in the months before presented to Animal Dentistry Referral Services for stomatitis.
Caudal mucositis noted mildly upon presentation = Feline Caudal Gingivostomatitis.
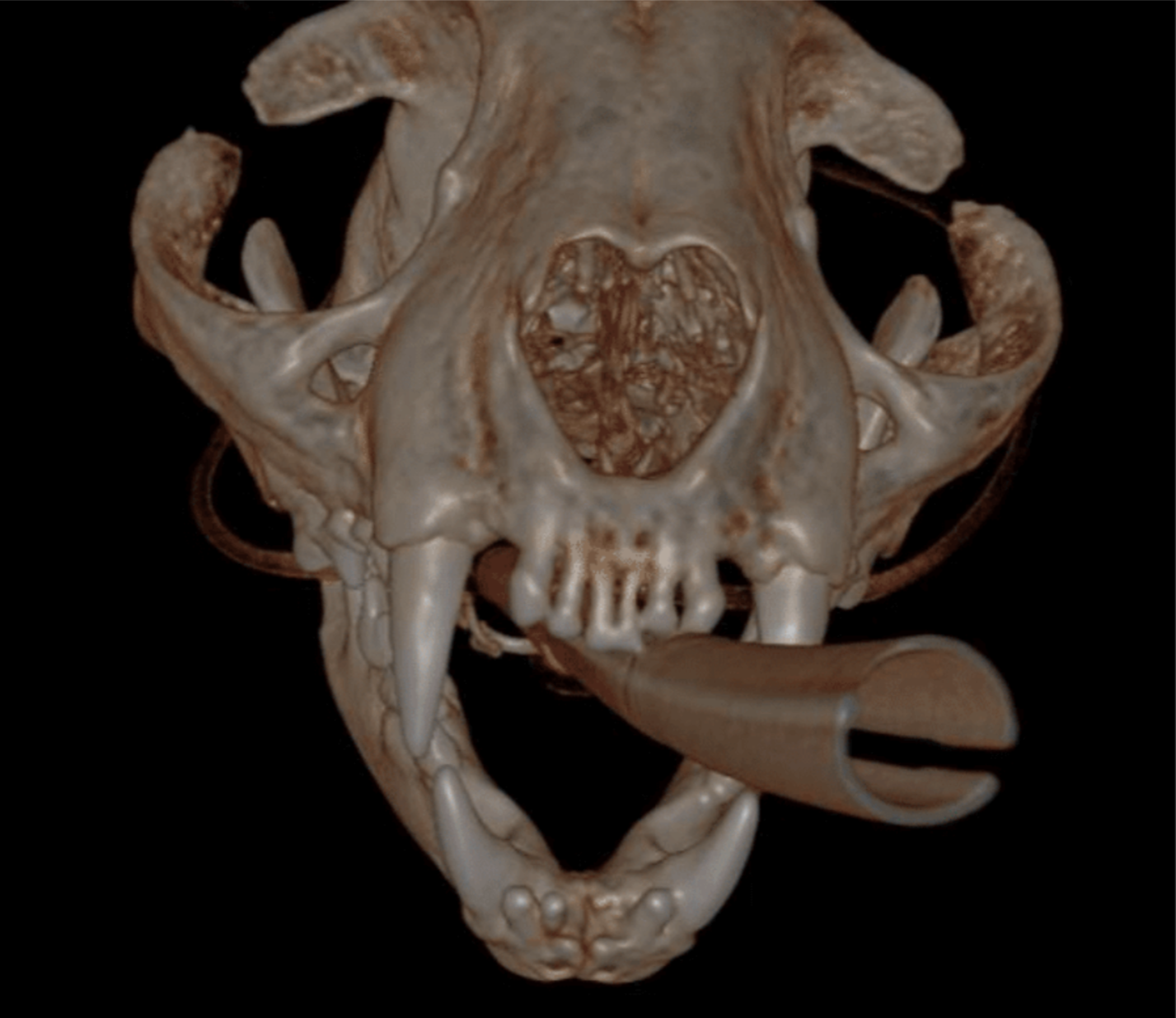
CBCT imaging revealed tooth resorption type 1 (inflammatory) on 409.
Below: Hard tissue reconstruction - 3D Overview

Below: High intensity CBCT overview

Below: (left) Front view (right) CT image of broken root - extracted

Below: Radiographs after mandibular extractions

FME performed as the sole curative treatment for FCGS. While not all cases are resolved by FME alone, none are cured without it. Typically, medical management is required before and after FME. Delayed FME after medical management often results in unsuccessful outcomes.
Extracted: 101-103, 201-203, 301-303, 401-403
Surgically Extracted: 104-109, 204-209, 304-309, 404-409 - 409 Type 1 resorption with root fracture noted.
The procedure involved envelope or small mesial triangle flaps per quadrant, with sectioning as needed. Retained tooth roots from the fracture of 409 were elevated and removed. Palatal/lingual tissue was released, along with the buccal flap. Margins were trimmed to healthy tissue, followed by alveoloplasty. Closure was achieved using 5-0 monofilament in a combination of simple interrupted, cruciate, and short continuous sutures. Additionally, horizontal mattress stitch was added to 104 and 204.
Below: Overview of both sides before extractions performed

Below: After extractions - Top jaw (maxilla)
.png?width=2092&height=600&name=After%20extractions%20-%20Top%20jaw%20(maxilla).png)
Below: After extractions - Lower jaw (mandible)
-2.png?width=940&height=265&name=After%20extractions%20-%20Lower%20jaw%20(mandible)-2.png)
Seven days post FME procedure, the patient returned for a feeding tube insertion due to reluctance to eat and signs of discomfort at home. The tube was placed, and feeding instructions were provided to the owner. Prednisolone and Doxycycline were prescribed during this visit. The patient responded well, and the feeding tube was removed, with the site healing within a month.
The patient now has a good appetite, and the feeding tube site had fully healed. He is playful and back to his normal self. However, he displayed anxiety during car rides, resulting in excessive drooling and resistance to examination of the back of his mouth. Due to the patient's comfort with his owner, it was decided to conduct the next evaluation in eight weeks, with the owner instructed to send a picture of the back of the patient's mouth.
Eight-weeks post-op, the patient's condition remained clinically excellent. His medication regimen was adjusted to prednisolone 1/2 twice weekly until completion (approximately 5.5 weeks), then discontinuation. Doxycycline dosage was reduced to once daily for four weeks, then twice weekly for another four weeks, with further adjustments based on the next eight-week update. Potential flares were anticipated around the six-week mark, and the owner was informed accordingly. The owner expressed satisfaction with the patient's progress and agreed to report any issues before the next evaluation.
An image was provided at the next eight-week mark, and the patient was able to discontinue Doxycycline and Prednisolone upon completing the prescribed course.
Case Summary: Guided Tissue Regeneration (GTR) is a technique performed to promote osseous regeneration, allowing for tissue growth (bone and soft...
%20-%20August%202024/3D%20image%20of%20open%20pulp%20chamber.jpg)
1 min read
Case Summary: In this case study, we examine a canine tooth that has been worn down to the pulp, leading to a painful exposure that allows bacteria...
%20Case%202%20-%20July%202024/Henry.jpeg)
1 min read
Case Summary: In this case study, we delve into the intricate treatment of a complicated crown fracture in a canine tooth, where the pulp is exposed,...